Hexobarbital
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Hexobarbital, Hexobarbitone, Methylhexabital, Methexenyl, Evipal |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | 25% |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.241 |
| Chemical and physical data | |
| Formula | C12H16N2O3 |
| Molar mass | 236.271 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| Density | 1.1623 g/cm3 |
| Melting point | 146.5 °C (295.7 °F) |
| Boiling point | 378.73 °C (713.71 °F) |
| Solubility in water | 0.435 mg/mL (20 °C) |
| |
| |
| (verify) | |
Hexobarbital or hexobarbitone, sold both in acid and sodium salt forms as Citopan, Evipan, and Tobinal, is a barbiturate derivative having hypnotic and sedative effects. It was used in the 1940s and 1950s as an agent for inducing anesthesia for surgery, as well as a rapid-acting, short-lasting hypnotic for general use, and has a relatively fast onset of effects and short duration of action.[1] Modern barbiturates (such as Thiopental) have largely supplanted the use of hexobarbital as an anesthetic, as they allow for better control of the depth of anesthesia.[2] Hexobarbital is still used in some scientific research.[3]
History
[edit]The chemical class of barbiturates are one of the oldest sedative-hypnotic agents known, dating back from the introduction of barbital in the early 20th century.[4] In Eastern Europe, hexobarbital (and other barbiturates) have been regularly used as drugs by pregnant women attempting suicide.[4] Hexobarbital was long thought to have potentially teratogenic and fetotoxic effects. The FDA has classified them as Pregnancy Category D or C.[5] Some research however, indicate that ingestion of Hexobarbital might cause congenital abnormalities.[4]
During World War II, Herta Oberheuser was a Nazi physician and convicted war criminal, investigating the effects of hexobarbital. The experiments were mostly performed on woman prisoners in the Ravensbrück concentration camp.
Application in research
[edit]Hexobarbital is used as the narcotic in the Hexobarbital Sleep Test (HST). HST identifies rodents with high or low intensity of microsomal oxidation, so fast (FM) or slow metabolizers (SM). The sleep test is for example used to predict the susceptibility and resistance to post-traumatic stress disorder (PTSD)[6] or to determine the effect of toxic compounds on sleep time.[7][8]
Synthesis
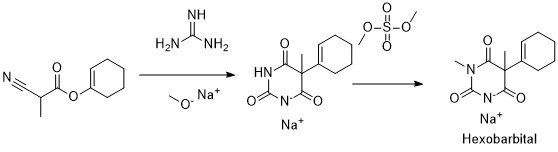
[edit]Hexobarbital can be synthesized by reacting cyclohex-1-enyl 2-cyanopropanoate with guanidine and sodium methylate. A hexobarbital sodium intermediate is then formed which can be methylated with dimethyl sulfate.[9]
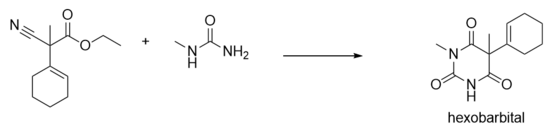
Another pathway for hexobarbital synthesis is reacting ethyl 2-cyano-2-(cyclohex-1-enyl)propanoate with N-methylurea.[10] This reaction is done in two stages, in the first stage the reactants are added with tert-butylate in tert-butyl alcohol at 20-50 °C. In the second stage hydrogen chloride is added with ethanol and water as solvent.
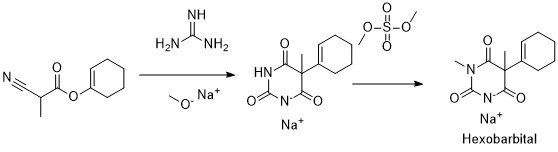
Synthesis of hexobarbital by reacting cyclohex-1-enyl 2-cyanopropanoate with guanidine and sodium ethylate, afterwards another methyl group is added through dimethyl sulfate 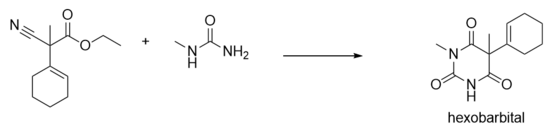
Alternative pathway for synthesis of hexobarbital by reacting ethyl 2-cyano-2-(cyclohex-1-enyl)propanoate with N-methylurea.
Reactivity
[edit]One of the cytochrome P450 isozymes is coded by the gene CYP2B1, where hexobarbital is the substrate. Hexobarbital and the isozyme can form an enzyme-substrate-complex through a hydroxylation reaction, which is involved in the metabolism of xenobiotics. the concentration of hexobarbital also plays a role in oxygenase and oxidase activity of hepatic microsomal cytochrome P450.[11]
Triacetyl oleandomycin, an inhibitor for isozyme CYP3A4, also inhibits hexobarbital metabolism and biological activity, indicating a close relationship between hexobarbital and cytochrome P450.[12]
Toxicity
[edit]Mechanism of actions
[edit]
The biological effects of hexobarbital depend primarily on its ability to penetrate the central nervous system.[13] Hexobarbital can potentiate GABAA receptors, like all barbiturates. It has been found over the years that the S(+) enantiomer of hexobarbital potentiates GABAA receptors more effectively than its R(-) enantiomer.[14] When GABA binds to the GABAA receptor, the chloride ion channels open such that chloride ions can flow into the neuron. This causes a hyperpolarization in the membrane potential of the neuron, which makes it less likely for the neuron to start an action potential. Therefore, this type of receptor is the major inhibitory neurotransmitter receptor in the mammalian central nervous system.[15] As a GABAA receptor potentiator, hexobarbital binds to the barbiturate binding site localized in the chloride ion channel, thereby increasing the binding of GABA and benzodiazepines to their respective binding site, allosterically.[16] Moreover, hexobarbital causes the chloride ion channel opening to their longest open state of 9 milli seconds, thereby causing the postsynaptic inhibitory effect to be extended.[14] In contrast to GABA, glutamate is the major excitatory neurotransmitter in the mammalian brain. In addition to the inhibitory effect, hexobarbital blocks, like all barbiturates, AMPA receptors, kainate receptors, neural acetylcholine receptors. And above all, barbiturates inhibit glutamate release by causing an open channel block on P/Q‐type high‐voltage activated calcium channels.[17] All in all, hexobarbital causes an CNS-depressant effect on the brain by inhibiting the glutamate release and potentiating the GABA-effect.
Metabolism
[edit]The hepatic metabolism of hexobarbital (HB) can be divided into different pathways all forming different metabolites.[18] The S(+) enantiomer of HB preferentially metabolizes into β-3'-hydroxyhexobarbital and the R(-) enantiomer preferentially metabolizes into α-3'-hydroxyhexobarbital, the reaction thus is stereoselective. Both enantiomers, however, form both α- and β-isomers. In total four enantiomers for 3'-hydroxyhexobarbital (3HHB) can be metabolized. This reaction is catalyzed by a cytochrome P450, CYP2B1.[19] All 3HHB isomers formed can undergo further metabolism via glucuronidation or dehydrogenation.
If 3HHB undergoes a glucuronidation reaction, via UDP-glucuronosyl transferases (UGTs), it is readily excreted. 3HHB can also undergo dehydrogenation, forming a reactive ketone, 3'-oxohexobarbital (3OHB). The biotransformation of 3HHB into 3OHB is via the enzyme 3HHB dehydrogenase (3HBD), a NAD(P)+ linked oxidation.[20] This enzyme is part of the aldo-keto reductase (AKR) superfamily. In humans, 3HBD has a high preference for NAD+.[19] These reactions are also stereospecific, the R(-) conformation preferentially forms 3OHB as 3HBD has the highest activity for this enantiomer in both alpha and beta form.[21]
New evidence proved the further metabolism of 3OHB into 1,5-dimethylbarbituric acid and a cyclohexenone glutathione adduct.[19] This biotransformation step takes place via an epoxide-diol mechanism.[22][23] The formation of a reactive epoxide, leads to the formation of the compounds mentioned.
Experiments in man indicated the major metabolites to be 3HHB, 3OHB and 1,5-dimethylbarbituric acid.[22]
Health effects in man
[edit]Excretion
[edit]The plasma half-life of HB in man is estimated at 222±54 min.[22] The clearance of HB differs between the two enantiomers and the age of the human subject. The clearance of the R(-) enantiomer is almost 10-fold greater than the clearance of the S(+) enantiomer. Clearance on average in elderly people, compared to young subjects, is slower.[24] Excretion is mainly via urine, for the three major metabolites.[19][22] The cyclohexenone glutathione adduct is excreted in the bile.[19]
Symptoms
[edit]An intoxication in man with hexobarbital can result in sluggishness, incoordination, difficulty in thinking, slowness of speech, faulty judgment, drowsiness or coma, shallow breathing and staggering. In some severe cases coma and death can be the result of an overdose.[18]
Effects on animals
[edit]The following table presents the studies about the effects of hexobarbital on animals, which are done in the 1900s. Most of these studies showed that hexobarbital has short-term toxicity effects and that it can induce hypnotic effects in mice, rabbits and frogs.
| Organism | Testtype | Route | Dose | Effect | Reference |
|---|---|---|---|---|---|
| rat | LD50 | intraperitoneal | 330 mg/kg (330 mg/kg) | [26] | |
| rat | LDLo | subcutaneous | 400 mg/kg (400 mg/kg) | [27] | |
| mouse | LD50 | oral | 468 mg/kg (468 mg/kg) | Prolongation of sleeping time | [28] |
| mouse | LD50 | intraperitoneal | 270 mg/kg (270 mg/kg) | Prolongation of sleeping time and immobility time, which are potentiated by L-asparagine | [29] |
| mouse | LDLo | subcutaneous | 250 mg/kg (250 mg/kg) | [30] | |
| mouse | LD50 | intravenous | 133 mg/kg (133 mg/kg) | Behavioural: somnolence (general depressed activity) | Archives Internationales de Pharmacodynamie et de Therapie., 163(11), 1966 |
| mouse | LDLo | intrapleural | 340 mg/kg (340 mg/kg) | Hypnotic effect, which is potentiated by 4,5-dihydro-6-methyl-2[2-(4-pyridyl)-ethyl]-3-pyridazinone (U-320) | [31] |
| mouse | LD50 | parenteral | 160 mg/kg (160 mg/kg) | Pharmacology and Toxicology. English translation of FATOAO., 20(569), 1957 | |
| rabbit | LDLo | oral | 1200 mg/kg (1200 mg/kg) | Ultra-short actors; hypnotic effect
Minimal lethal dose: 1200 mg/kg Minimal hypnotic dose: 15 mg/kg |
[32] |
| rabbit | LDLo | intravenous | 80 mg/kg (80 mg/kg) | Ultra-short actors; hypnotic effect
Minimal lethal dose: 80 mg/kg Minimal hypnotic dose: 15 mg/kg |
[32] |
| rabbit | LDLo | rectal | 175 mg/kg (175 mg/kg) | Ultra-short actors; hypnotic effect
Minimal lethal dose: 175 mg/kg Minimal hypnotic dose: 15 mg/kg |
[32] |
| frog | LDLo | intraperitoneal | 30 mg/kg (30 mg/kg) | [33] | |
| frog | LD50 | parenteral | 148 mg/kg (148 mg/kg) | Pharmacology and Toxicology. English translation of FATOAO., 20(569), 1957 |
In popular culture
[edit]In Agatha Christie's 1937 mystery Cards on the Table, Hexobarbital is used in conjunction with Veronal to induce overdose. It is referred to by Hercule Poirot as both N-methyl-cyclo-hexenyl-methyl-malonyl urea and Evipan.[34]
References
[edit]- ^ Lexikon der Neurowissenschaft: Hexobarbital (in German)
- ^ Pubchem. "Hexobarbital | C12H16N2O3 - PubChem". pubchem.ncbi.nlm.nih.gov. Retrieved 2016-05-02.
- ^ Tseilikman VE, Kozochkin DA, Manukhina EB, Downey HF, Tseilikman OB, Misharina ME, Nikitina AA, Komelkova MV, Lapshin MS, Kondashevskaya MV, Lazuko SS, Kusina OV, Sahabutdinov MV (April 2016). "Duration of hexobarbital-induced sleep and monoamine oxidase activities in rat brain: Focus on the behavioral activity and on the free-radical oxidation". General Physiology and Biophysics. 35 (2): 175–83. doi:10.4149/gpb_2015039. PMID 26689857.
- ^ a b c Timmermann G, Czeizel AE, Bánhidy F, Acs N (2008-02-01). "A study of the teratogenic and fetotoxic effects of large doses of barbital, hexobarbital and butobarbital used for suicide attempts by pregnant women". Toxicology and Industrial Health. 24 (1–2): 109–19. Bibcode:2008ToxIH..24..109T. doi:10.1177/0748233708089004. PMID 18818187. S2CID 36948994.
- ^ "FDA Pregnancy Categories - CHEMM". chemm.nlm.nih.gov. Archived from the original on 2021-08-27. Retrieved 2021-02-27.
- ^ Komelkova M, Manukhina E, Downey HF, Sarapultsev A, Cherkasova O, Kotomtsev V, Platkovskiy P, Fedorov S, Sarapultsev P, Tseilikman O, Tseilikman D, Tseilikman V (August 2020). "Hexobarbital Sleep Test for Predicting the Susceptibility or Resistance to Experimental Posttraumatic Stress Disorder". International Journal of Molecular Sciences. 21 (16): 5900. doi:10.3390/ijms21165900. PMC 7460591. PMID 32824478.
- ^ Bornheim LM, Borys HK, Karler R (March 1981). "Effect of cannabidiol on cytochrome P-450 and hexobarbital sleep time". Biochemical Pharmacology. 30 (5): 503–7. doi:10.1016/0006-2952(81)90636-5. PMID 7225146.
- ^ Schnell RC, Prosser TD, Miya TS (May 1974). "Cadmium-induced potentiation of hexobarbital sleep time in rats". Experientia. 30 (5): 528–9. doi:10.1007/BF01926332. PMID 4833683. S2CID 6402325.
- ^ VCH Publishers (2002). Ullman's encyclopedia of industrial chemistry. Wiley-VCH. OCLC 50618230.
- ^ US 2015376136, Chumakova L, Patron A, Priest C, Karanewsky D, Kimmich R, Clayton B, Jeffrey B, Hammaker R, Chumakov V, Zhao W, Noncovich A, Ung J, "Compounds useful as modulators of trpm8", published 31 December 2015, issued 12 December 2017, assigned to Senomyx Inc
- ^ Heinemeyer G, Nigam S, Hildebrandt AG (November 1980). "Hexobarbital-binding, hydroxylation and hexobarbital-dependent hydrogen peroxide production in hepatic microsomes of guinea pig, rat and rabbit". Naunyn-Schmiedeberg's Archives of Pharmacology. 314 (2): 201–10. doi:10.1007/BF00504539. PMID 7453835. S2CID 37489777.
- ^ Timbrell JA (2009). Principles of biochemical toxicology. Informa Healthcare. p. 181. ISBN 978-0-8493-7302-2. OCLC 243818515.
- ^ Andrews PR, Mark LC (October 1982). "Structural specificity of barbiturates and related drugs". Anesthesiology. 57 (4): 314–20. doi:10.1097/00000542-198210000-00014. PMID 6751157.
- ^ a b Yamakura T, Bertaccini E, Trudell JR, Harris RA (2001-04-01). "Anesthetics and ion channels: molecular models and sites of action". Annual Review of Pharmacology and Toxicology. 41 (1): 23–51. doi:10.1146/annurev.pharmtox.41.1.23. PMID 11264449.
- ^ Sigel E, Steinmann ME (November 2012). "Structure, function, and modulation of GABA(A) receptors". The Journal of Biological Chemistry. 287 (48): 40224–31. doi:10.1074/jbc.R112.386664. PMC 3504738. PMID 23038269.
- ^ Olsen RW, Sapp DM, Bureau MH, Turner DM, Kokka N (1991). "Allosteric actions of central nervous system depressants including anesthetics on subtypes of the inhibitory gamma-aminobutyric acidA receptor-chloride channel complex". Annals of the New York Academy of Sciences. 625: 145–54. doi:10.1111/j.1749-6632.1991.tb33838.x. PMID 1711804. S2CID 12448489.
- ^ Löscher W, Rogawski MA (December 2012). "How theories evolved concerning the mechanism of action of barbiturates". Epilepsia. 53 Suppl 8 (s8): 12–25. doi:10.1111/epi.12025. PMID 23205959. S2CID 4675696.
- ^ a b "Hexobarbital". go.drugbank.com. Retrieved 2021-03-08.
- ^ a b c d e Takenoshita R, Toki S (December 2004). "[New aspects of hexobarbital metabolism: stereoselective metabolism, new metabolic pathway via GSH conjugation, and 3-hydroxyhexobarbital dehydrogenases]". Yakugaku Zasshi. 124 (12): 857–71. doi:10.1248/yakushi.124.857. PMID 15577260.
- ^ Endo S, Matsunaga T, Matsumoto A, Arai Y, Ohno S, El-Kabbani O, Tajima K, Bunai Y, Yamano S, Hara A, Kitade Y (November 2013). "Rabbit 3-hydroxyhexobarbital dehydrogenase is a NADPH-preferring reductase with broad substrate specificity for ketosteroids, prostaglandin D₂, and other endogenous and xenobiotic carbonyl compounds". Biochemical Pharmacology. 86 (9): 1366–75. doi:10.1016/j.bcp.2013.08.024. PMID 23994167.
- ^ Furner RL, McCarthy JS, Stitzel RE, Anders MW (October 1969). "Stereoselective metabolism of the enantiomers of hexobarbital". The Journal of Pharmacology and Experimental Therapeutics. 169 (2): 153–8. PMID 5824599.
- ^ a b c d Vermeulen NP, Rietveld CT, Breimer DD (April 1983). "Disposition of hexobarbitone in healthy man: kinetics of parent drug and metabolites following oral administration". British Journal of Clinical Pharmacology. 15 (4): 459–64. doi:10.1111/j.1365-2125.1983.tb01530.x. PMC 1427803. PMID 6849782.
- ^ Takenoshita R, Nakamura T, Toki S (August 1993). "Hexobarbital metabolism: a new metabolic pathway to produce 1,5-dimethylbarbituric acid and cyclohexenone-glutathione adduct via 3'-oxohexobarbital". Xenobiotica; the Fate of Foreign Compounds in Biological Systems. 23 (8): 925–34. doi:10.3109/00498259309059419. PMID 8284947.
- ^ Smith DA, Chandler MH, Shedlofsky SI, Wedlund PJ, Blouin RA (December 1991). "Age-dependent stereoselective increase in the oral clearance of hexobarbitone isomers caused by rifampicin". British Journal of Clinical Pharmacology. 32 (6): 735–9. doi:10.1111/j.1365-2125.1991.tb03982.x. PMC 1368555. PMID 1768567.
- ^ PubChem. "Hexobarbital". pubchem.ncbi.nlm.nih.gov. Retrieved 2021-03-07.
- ^ Klinger W (March 1970). "[Toxicity, narcotic effect, blood level after awakening, elimination from the blood and biotransformation of hexobarbital in rats of different ages after induction with barbital and carbon tetrachloride poisoning]". Archives Internationales de Pharmacodynamie et de Therapie. 184 (1): 5–18. PMID 5448769.
- ^ "Naunyn-Schmiedeberg's Archives of Pharmacology | Volumes and issues". SpringerLink. Retrieved 2021-03-09.
- ^ Reinhard JF, Kimura ET, Scudi JV (December 1952). "Pharmacologic characteristics of 1-(ortho-toluoxy)2, 3-bis-(2, 2, 2-trichloro-1-hydroxyethoxy)-propane". The Journal of Pharmacology and Experimental Therapeutics. 106 (4): 444–52. PMID 13023555.
- ^ Forney RB, Hughes FW, Richards AB, Gates PW (November 1963). "Toxicity and depressant action of ethanol and hexobarbital after pretreatment with asparagine". Toxicology and Applied Pharmacology. 5 (6): 790–3. Bibcode:1963ToxAP...5..790F. doi:10.1016/0041-008X(63)90071-1. PMID 14082484.
- ^ Irrgang K (June 1965). "[On the pharmacology of 5-ethyl-5(3-hydroxyisoamyl)-barbituric acid--a breakdown product of 5-ethyl-5-isoamyl-barbituric acid]". Arzneimittel-Forschung. 15 (6): 688–91. PMID 5899249.
- ^ Buller RH, Rockhold WT, Buzard JA, Stern IJ (1961-10-01). "The Potentiating Effect of 4,5-Dihydro-6-Methyl-2[2-(4-Pyridyl)-Ethyl]-3-Pyridazinone (u-320) on Hexobarbital Hypnosis". Journal of Pharmacology and Experimental Therapeutics. 134 (1): 95–99. ISSN 0022-3565.
- ^ a b c Werner HW, Pratt TW, Tatum AL (1937-06-01). "A Comparative Study of Several Ultrashortacting Barbiturates, Nembutal, and Tribromethanol". Journal of Pharmacology and Experimental Therapeutics. 60 (2): 189–197. ISSN 0022-3565.
- ^ Tatum AL (October 1939). "The present status of the barbiturate problem". Physiological Reviews. 19 (4): 472–502. doi:10.1152/physrev.1939.19.4.472.
- ^ Christie A (1937). Cards on the Table. New York: William Morrow. p. 242. ISBN 978-0-06-207373-0.